The Vegan Cardiologist on a Mission to Prevent Million Heart Attacks - Meet Dr Joel Kahn
Do you know how much protein your body actually needs on a day-to-day basis? Could you name 3 symptoms of an impending heart attack? If you have a history of heart disease in your family, do you know which preventative tests to ask your doctor for? Find out the answers to these questions and so much more in our riveting interview with Dr Joel Kahn.
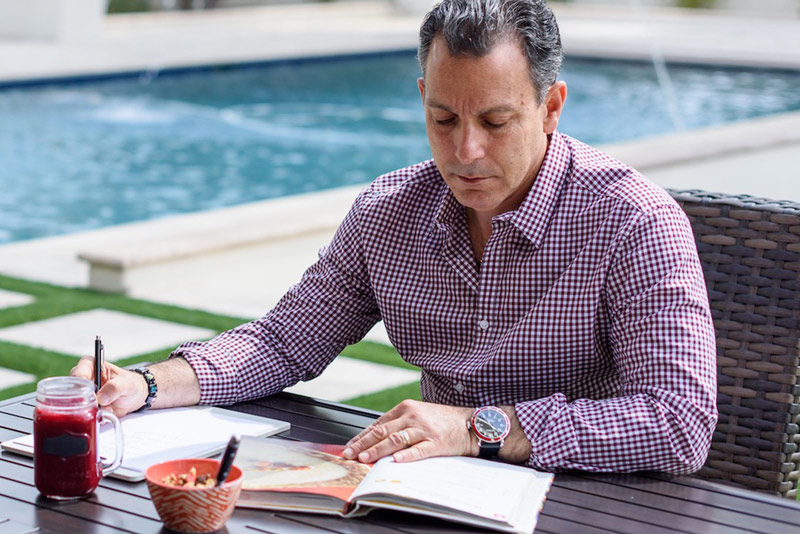
What do you get when you combine veganism, cardiology and prevention? You get a holistic cardiologist passionate about the health benefits of a plant-based, anti-ageing diet. Join us in learning more about Dr Kahn and the different ways we can better our longevity without falling for pseudoscience.
Dr Kahn, seeing how your goal is to prevent 1 million heart attacks, what tips do you most often give to patients looking to improve their cardiovascular health?
As you know, the number one cause of death in the world for both men and women is cardiovascular disease, which is a fancy term for heart attacks, strokes, ruptured aneurysms, and basically sick arteries.
And if you stop and think about it, at least from my experience as a cardiologist for over 30 years in the United States, we have a very odd system. We screen people for cancer regularly. Patients get suggestions to get a colonoscopy, a mammogram, perhaps a cervical exam, or a prostate exam. But if you think about what we do to screen for the number one cause of death in the world - sudden cardiac death, heart attacks, and strokes, we do essentially nothing.
Hopefully, you check your blood pressure. And that is my number one tip for preventing heart attacks. Get a home blood pressure cuff, put it on your coffee table and use it every day. It's worthless if you have it sitting in the drawer or the closet like everybody does. And even more useless if you don't own one. You might get your blood work done, but doctors are still doing the same blood work they did 30 years ago.
They're not getting inflammation markers like high-sensitivity C-reactive protein. They're probably not getting a vitamin D level and Omega-3 level test for genetic cholesterol. And finally, you know, a colonoscopy looks at the colon, a mammogram, looks at the breast. We do nothing. We're not even allowed in the United States to order a routine electrocardiogram anymore, which is a really poor test to detect silent heart disease.
I want to stress, that we can diagnose heart disease ten years before a heart attack, and five years before a stroke. We can diagnose abnormalities of the carotid arteries and other predisposing factors for stroke. We can detect these things, but we don't have a program. So I tell my patients to get a home blood pressure cuff (I use a hashtag on social media #testnotguess).
The most efficient, cost-effective, and reasonable way to test is with a CT scan of the heart called a coronary artery calcium scan available worldwide since 1990. It’s very easy, and inexpensive, with no IV, no injection, and no allergies to medication because there are no medications. And basically, in about five seconds, a CT imaging picture is made of the heart and the heart arteries.
You get a ton of information. You find out if your lungs are healthy. You find out if your aorta is normal or enlarged and there are some people that drop dead from an enlarged aorta. But the key finding is, are my heart arteries ageing, are they calcified? It's silent, but it can be deadly. And if we're going to stop a million heart attacks, we need to start teaching people at age 40 or 45 that they should ask for extra blood work.
They should ask for a heart calcium CT scan, which is an inexpensive test. In some places in the United States, it's covered through insurance. You should insist that you get these and then repeat them on a regular basis, just like we repeat, a mammogram and a colonoscopy. The cost isn’t actually what’s stopping people from preventing heart disease. It's this lethargic approach to heart disease. And it's inexcusable because these are not brand-new tests.
That is so important and definitely something I should encourage people around me to do. For decades now, researchers have been engaging in the big cholesterol debate. What can you tell us about this? Is there such a thing as good and bad cholesterol, and are we genetically predisposed to it or can we change it with dietary interventions?
There's actually no cholesterol debate. There's cholesterol misinformation, and I hate to use that term. There are such massive data points. It goes back to 1985 when the Nobel Prize in Medicine was awarded to Dr Brown and Dr Goldstein for exploring what is called LDL cholesterol receptors in the liver.
I was in Dallas, Texas, when all that was going on, I had just begun my cardiology training. And from 1985 to the present there are thousands and thousands of studies that indicate there's not just an association between a high LDL cholesterol and developing clogged arteries and events like strokes and heart attacks, it's causative. It's actually in the plaque. It incites inflammation.
There is no debate. Of course, there's a noisy group out there because there always have to be exceptions. And one has to understand that cholesterol is a risk factor, not the risk factor. There are at least 25 known risk factors and some people actually put down 400 for developing heart disease.
So, yes, you could have normal LDL cholesterol and have a heart attack. There are smokers that don't get lung cancer. There are people who never wear a seatbelt and don't die in a car accident. That doesn't mean you don't wear a seatbelt, doesn't mean you encourage smoking. The rule is still there, so there's no debate about it.
The average LDL cholesterol until teen years is often 25 to 30 unless you're on a typical American garbage diet, then it's going to rise. During the biggest growth period in humans, which is childhood, we have very low LDL cholesterol traditionally and are usually on good diets.
Our brains develop, our nerves develop and our hormones develop. We go through puberty and then suddenly, we start becoming lethargic and sitting in chairs at school and we eat poorly and our cholesterol goes up and up and up. So it looks like you probably need an LDL cholesterol around 25 to support a healthy metabolism, including brain health because the brain has its own cholesterol synthesis system.
So if your blood LDL cholesterol is 25, it doesn't mean you're deficient in your brain. Kids proved the point. Kids' brains make cholesterol. Adults’ brains make cholesterol separate from the liver and other synthetic sites of cholesterol. And there is an increasing body of data. There are genetic variations where you run a low cholesterol your whole life and the biggest side effect of a low cholesterol is fewer heart attacks, fewer strokes, and a longer lifespan.
We used to say LDL cholesterol, low-density lipoprotein is lousy. It's lousy if it's above 25 to 50 milligrams per deciliter because you don't need it that high. You might not develop heart disease, but you might. HDL cholesterol - high-density lipoprotein, we used to call H equals happy. Low is bad. High is good. The last decade has completely destroyed that simple approach because we know that there's a sweet spot.
An LDL may be between 50 and 80 is most associated with the absence of atherosclerosis. A low HDL is still associated with atherosclerosis, but so is a high HDL, particularly in men. Men with an HDL over 80 just statistically have an increased risk of silent atherosclerosis that could result in stroke or sudden death.
So I think all the efforts so far to work on HDL, with the exception of obviously a healthy diet, regular exercise and maybe a glass of red wine here and there have largely failed.
At least 30 years ago I lectured side by side with Dr Thomas Dayspring, who's an internationally known cholesterol expert, and he kept saying a strange statement - It's an ApoB world, boys and girls.
And it turned out that's all you need to know. It's an ApoB world, boys and girls, and be sure to check it and lower it in people who have evidence of silent or clinically evident atherosclerosis.
There are patients in my practice that I've checked their arteries, I've checked their heart, I've checked their peripheral arteries. They have no atherosclerosis. I’ll check it out and recheck them in a few years. So I don't treat those people necessarily, I certainly don't put them on prescription medication.
Year after year, the World Health Organization chooses the Mediterranean diet as the healthiest one. Seeing how this is a plant-based diet, a lot of people would immediately ask if they would have enough protein with it. What is the actual daily serving of proteins for a regular person and why do we think of them as the most important nutrient?
The World Health Organization picked the Mediterranean diet as the best example. Actually recently in the United States, the American Heart Association picked a version called the DASH diet because it promotes lower salt. And that's more consistent with the American heart guidelines.
But right below the DASH diet is the Mediterranean diet, and I'm all in favour of the Mediterranean diet. I do it plant-based. I stopped eating every animal product when I was 18 years old, so 46 years ago. So I’m a living, breathing, long-term vegan, long-term whole food, plant-based eater, and a healthy one.
No prescription drugs, no surgeries, excellent health, pretty low GlycanAge. And I think the diet is a part of it. You know, I give the most credit for intelligent discussions of nutrition to the University of Southern California scientists.
Dr Valter Longo has done research with another ageing expert, Morgan Levine, PhD that suggests from animal models and then human studies, that a low protein diet is actually an advantage until your older years, you're less likely to stimulate pathways that increase mTOR activity, increase IGF-1 levels, promote cancer, maybe promote atherosclerosis.
So he actually recommends 0.4g/kg of protein until you're in your mid to late 60s, which I'm getting pretty close to. That's half of what the US government recommends. They recommend 0.8, and Dr Longo says in your mid to late 60s, you should increase the protein intake, but also lift some weights, get in the gym, and do some push-ups.
My biggest source of protein is legumes. I know that there's a debate about legumes and lectins, another misinformation campaign, this time from Steven Gundry and his book Plant Paradox that completely confused the world.
You know, there's data that if you're older and you eat legumes, you have a side effect. It's called more longevity. That's actually published research. If you study Dan Buettner and his five blue zones around the world, legumes are the most common food in people that live to a healthy age, to late 90s or over 100. Dr Longo teaches the same.
His recipes often feature lentils. I can tell you his own dinner is typically a lentil-based dinner. So is mine. I've interviewed him about his typical daily diet, a very Mediterranean, plant-based diet. It works out well. And if you lower protein and lower added sugar in the diet, the exception being whole fruit, which is always a good thing to eat, you will impact pathways that promote ageing, including arterial vascular, and cardiac ageing.
But if you're getting in your late 60s and 70s and you're getting frail, you know, open another can of chickpeas, eat some more green beans and green peas. Eat every kind of lentil under the planet and don't fear the plant paradox. That's all nonsense.
Do men and women experience the same heart attack symptoms and what are they?
That’s a great question. Many do experience the same symptoms. By that I mean, the classic symptoms I’ve seen in so many people in my career, which included a long period when I was an interventional cardiologist. So I was the one at the bedside at the heart attack, ready to reopen the artery with the emergency procedure.
Is there ever a person whose cardiac symptoms before and during a heart attack are predominantly shortness of breath? Yes. Occasionally just extreme nausea and stomach upset? Yes.
One of the arteries to the heart that frequently causes a heart attack is called the right coronary artery. And it travels down to the bottom of the heart. And basically, the stomach is sitting right there, right below it. And there's a lot of shared nerve supply between the stomach and the bottom of the heart. So if you get a heart attack involving that artery towards its distal termination, sometimes people think they’re having bad heartburn and it can be very tragic.
They delay approaching the emergency room and could even die. So occasionally it's just a sudden intense stomach distress and burning that shouldn’t be ignored. Women may have more of the atypical symptoms. They may not have that classic one we call angina, also they may not have a couple of weeks of warning. They just may be tired with some palpitations.
They may be winded where they haven't winded a month ago. They may have some of that burning. So never ignore a new symptom, particularly if it's coming on with exertion, like working out or cleaning the house.
The thing about women, on average, if a woman isn't a heavy smoker or a type one diabetic, and doesn't have a genetic cholesterol disorder, she will develop heart disease about 12 years later than men. So men may have that heart attack at 54 and women who've been in menopause for a decade at age 66. But there are so many exceptions to the rule.
There are a lot of reasons to believe that menopause triggers changes and that having periods is associated with a full complement of female hormones. It's rather good for the lining of your arteries. It favours better sleep, better weight, better glucose control, and better cholesterol control. A lot of lab values worsen during and after menopause, including blood cholesterol.
So the metabolic system becomes more abnormal. Now, women may get on well-done hormone replacement therapy early in menopause. It gives them a good chance to avoid that otherwise delayed cardiac ageing process that they're going to run into.
Can you tell us which supplements you recommend for longevity? And is there such a thing?
It’s such a challenging concept. Because there's many that could be put there. There are some that have no data, there are some that have animal data. But it still depends on the individual. I think one that gets ignored a lot is Coenzyme Q10, sometimes called Ubiquinone or the other version called Ubiquinol. There is solid data on this supplement.
Number one, CoQ10 is hard to get from the diet. Number two, it's clearly known that the body starts to make less of it with age over 40 and it makes way less of it if you're taking a cholesterol medication called statin. So you end up being CoQ10 deficient. I don't have one patient in my practice on a statin who isn't also taking CoQ10. They have to. It has to be together.
Not that we have all the data in the world, but we have good data and there's actually even a new supplement for people on statins that may return their metabolism to optimal called geranylgeranyl.
I use a supplement that has both CoQ10 and geranylgeranyl together in one pill. For CoQ10, there's a nice randomized study in Sweden of people aged 70 and up. Healthy people were put on CoQ10 and Selenium or a placebo. And although I think the study went for five years, they've now followed these people for 14 years. There's a rather dramatic advancement or an advantage to being on the combination.
And in Sweden, I believe the soil is selenium deficient. So in the United States, I usually just use CoQ10 alone. There's some recent conversation that taurine is an amino acid that does help to lower blood pressure. Naturally, a lot of my patients take it for that reason. Taurine can be difficult to get on a plant-based diet. So I've encouraged my patients to supplement with 1000mg of taurine, sometimes higher if they have high blood pressure.
But definitely check your vitamin D level and supplement it. I think it's crucial to check your omega-three blood level. Then you get into some of the new ones that I think have exciting data. There's a combination that I don't hear many people talk about called Glycine GlyNAC. It helps support the production of glutathione. There are both animal data and small human studies on the elderly that people taking NAC have better muscle strength, avoid frailty, and better cognitive function. Can't really say for sure. It looks to extend healthspan. It's inexpensive and it's safe.
Then you get to some of the others. I'm optimistic about Spermidine, which you can eat in wheat germ. It’s another example where whole grains are healthy for you, but the wheat germ is rich in Spermidine, and so are green peas, mushrooms and tofu. Spermidine is available in a capsule form and there's pretty good data for brain function, cognitive function and at least in animal models, longevity.
And in that same vein, there's a relatively new one called Urolithin A, which comes from pomegranates. And there are human studies that show improved mitochondrial function called mitophagy that may improve exercise performance. I think it's a stretch to say it is known to support longevity, but I think it's reasonable to consider that.
Obviously, I'm interested in metformin. I still think we need more data before every human on the planet takes metformin. I'm interested in rapamycin. I'm in a randomized study myself. I'm a volunteer subject where I'm taking a pill a week that's either a placebo or ten milligrams of rapamycin. I'll find out at the end of the year.
But at the end of the day, I think the best supplement for longevity is to check your heart. A recent large study says - I don't care if you feel good. I don't care if you say you don't have heart disease. If your calcium score is over 300, you basically have the same risk of dying in the next ten years as somebody who's already had a heart attack.
So you got to get on treatment. You got to get on the Mediterranean diet or the DASH diet or a plant-based one. Get to the gym and get your sleep. I would put sleep as maybe the most important longevity supplement.
Actually, you know, the American Heart Association used to teach something called the Life’s Essential Seven or Simple Seven. Now it's Life’s Essential Eight because they added the critical role of sleep. And I think there's enough data to suggest if you have sleep apnea, it's going to shorten your lifespan.
If you sleep four hours a night because you have bad dreams or a bad schedule, or you watch YouTube till three in the morning like so many of my patients, you’re engaging in life-shortening activities. So I spend a tremendous amount of time with patients trying to get them 7 to 8 hours of good quality sleep, track their sleep, and treat their sleep apnea.
But when it comes to supplements, you should start slowly. There is this very interesting case study going on of Brian Johnson, who's been spending $2 million a year. And he's got plenty of money to spend at age 45. And I recently saw that he takes 76 or 80 supplements a day and it's an interesting list.
Acarbose is first on the list. I don't take Acarbose, because I need to study that up more. He does a lot of spirulina and I think a fair amount of chlorella. And those are actually foods. It isn't really fair to call it a supplement. So there is still a lot of research to be done in this field.
What first attracted you to GlycanAge?
I'm a big social media guy and you have a wonderful Instagram page. I’m in this rapamycin study where I have to do a GlycanAge test as a baseline at six months and at 12 months. So that's part of the research study. I think they chose wisely. I think you are the best age assessment test.
I would still do a heart test, don't forget. And my heart at the age of 64, is as clean as you're going to find on the planet. That's years of long and hard work and not medication. I've done some of the other epigenetic ageing tests. I've done telomere tests in the past. I don't do them a lot, but I just think GlycanAge is fascinating.
Your podcast is educational, your research is excellent. You know, the whole field of glycans is really rich in literature, but it just isn't talked about much because there hasn't really been a decent way to assess the process.
My first GlycanAge before the research study was actually 20 and I was 63 years old. Now it's for some reason 23 on repeat. I don't know what it means. I don't feel 20 years old every day, but it's good stuff, it's an important test. I had actually bought a kit before this rapamycin trial. I just never had gotten around to doing it. So I have been researching your company for the last year and a half and I just have to say - keep up the good work.
Find out more about Dr Kahn here.