Vitamin D3's Role in Chronic Disease Prevention
Learn why Vitamin D3 is essential for optimizing health and managing diseases like cancer and diabetes.

Discover the power of the sun! AKA.. vitamin D3.
The Vitamin D3 Deficiency Pandemic
We are currently living in an era where people are spending less and less time outdoors. As a result, vitamin D3 deficiency is on the rise. What does this mean for our health? This article will delve into the central and extensive role of vitamin D3, and emphasise the detriment lack of sunlight has on the human body. However, it’s not all doom and gloom (no pun intended). Luckily, vitamin D3 supplementation is inexpensive, readily accessible and provides a boost of the sunshine vitamin even on a rainy day!
We have previously covered how vitamin D3 synergizes with vitamin K2 to promote bone health (read here). But did you know, although vitamin D3 is essential for strong bones, it is also utilized to regulate a vast network of biological functions including inflammation and even the prevention of some cancers? But first, what is vitamin D3 and how does the sun create it?
What Is Vitamin D3 and How Is It Produced?
In humans, vitamin D3 is produced within the deep layers of the skin in response to sunlight exposure. This is because the sun’s UVB rays destabilize a cholesterol component within the skin to form pre-vitamin D. Then, following sun exposure, pre-vitamin D spontaneously rearranges its atoms to form vitamin D3. In addition, vitamin D3 can be ingested through diet in foods such as eggs or by supplementation.
Intriguingly, vitamin D3 must be processed by the liver, followed by the kidneys to form the active compound responsible for its effects. Hereafter, when referring to the effects of vitamin D3, this describes the effects of vitamin D3 following its metabolism.
The cellular response to vitamin D3 is mediated by the Vitamin D Receptor (VDR), which is found in a vast array of cell types including muscle, fat, immune and even cancer cells. Here, vitamin D3 binds tightly to VDR resulting in its activation. Once activated, VDR binds to distinct sequences in the DNA, resulting in vitamin D-dependent activation of specific genes. VDR has been shown to be expressed in as many as 1000 different cell types and modulate the expression of 1000+ genes. This genetic blueprint therefore explains why vitamin D3’s effects within the body are far-reaching and extensive.
Interestingly, vitamin D3 supplementation has gained traction for its potential to prevent certain chronic diseases. Here, we will delve into the role of vitamin D3 supplementation and its emerging role in obesity, diabetes, inflammation and cancer.
Vitamin D3's Role in Obesity and Weight Loss
Obesity is a leading risk factor for cardiovascular disease, atherosclerosis and diabetes. Interestingly, observational studies have demonstrated obesity and vitamin D3 deficiency are positively correlated. Based on these findings, it’s therefore no surprise that vitamin D3 supplementation for weight loss has been a topic of extensive research.
Can Vitamin D3 Help with Weight Loss?
Restoring vitamin D3 levels in vitamin D3 deficient, obese individuals has been suggested to promote weight loss. Specifically, several studies have demonstrated that vitamin D3 may promote fat loss when combined with lifestyle interventions. This was demonstrated by a study where women who were assigned a calorie deficit + vitamin D3, had lower triglycerides after 12 months versus the calorie deficit only-group. Intriguingly, a study assessing the effects of vitamin D3 on body composition in obese adults, showed that although vitamin D3 did not result in weight loss, individuals following the vitamin D3 intervention lost significantly more visceral fat compared to the placebo group. Thus, suggesting vitamin D3 may play a role in fat loss specifically.
Emerging data suggests that vitamin D3 supplementation may help with fat loss indirectly through the regulation of several physiological processes. How?

Regulation of Hunger Hormones
Leptin is a hunger hormone responsible for stimulating satiety. Obese individuals often display dysregulated hunger hormones which can lead to excessive eating. Interestingly, a recent study involving >6,000 participants, found individuals with low vitamin D3 levels also had low levels of leptin. In fact, increased vitamin D3 levels have been shown to positively impact leptin production at the cellular level by activating the expression of the leptin gene LEP. Therefore, taken together, this suggests that vitamin D3 may influence weight management indirectly through regulating the hunger hormone leptin.
Reduction of Pro-inflammatory Adipokines
Another mechanism by which vitamin D3 may help with fat loss is through the reduction of inflammation. Specifically, the vitamin D receptor VDR, has been shown to dampen the expression of genes that code for adipokines. These are pro-inflammatory cytokines that promote the synthesis of fat cells. Therefore, when vitamin D3 is abundant, it can prevent fat-gain by inhibiting pro-inflammatory pathways. Again, this highlights why vitamin D3 sufficiency may be important for maintaining a healthy weight.
Promoting Thyroid Health
Hypothyroidism (an underactive thyroid) can lead to weight gain if not properly managed, and can be exacerbated by vitamin D3 deficiency. Interestingly, one study revealed that subjects with sub-clinical hypothyroidism when given a vitamin D3 supplement for 6 months, exhibited improved thyroid function following the regimen. These results have been mirrored in several randomized controlled trials. As such, one study found that vitamin D3 supplementation improved thyroid function in both men and women in only 12 weeks! This suggests that vitamin D3 may help to maintain a healthy weight indirectly by promoting the proper thyroid function.
Together, these studies emphasize how vitamin D3, and thus adequate sun exposure, may help with weight management by balancing hunger hormones, reducing inflammation and promoting a healthy thyroid.
Vitamin D3 and Its Preventative Role in Diabetes
Diabetes Mellitus (Diabetes) is a disorder that affects the body’s ability to regulate blood sugar due to insulin deficiency. Individuals with Type 1 Diabetes exhibit a complete loss of insulin due to the auto-immune destruction of insulin-producing beta-cells. In this case, people with Type 1 Diabetes are typically genetically predisposed to developing the disorder, and require exogenous insulin to manage the condition. In contrast, Type 2 Diabetes is defined by a gradual and increasing insensitivity to insulin, leading to hyperglycaemia (high blood sugar). The development of Type 2 diabetes is at large attributed to lifestyle factors such as obesity and a sedentary lifestyle, and can be reversed with interventions such as Metformin.
Vitamin D3 deficiency is recognized as a risk factor for Type 2 diabetes, based on the observation that there is a positive correlation between Type 2 diabetes and low vitamin D3 levels. Interestingly, studies have shown that supplementing with vitamin D3 can help to prevent pre-diabetes from developing into new-onset Type 2 diabetes in 11% of individuals. In addition, vitamin D3 supplementation has been shown to significantly reduce fasting blood glucose and improve insulin sensitivity in both healthy and obese individuals. These results show the potential for vitamin D3 to prevent and even reverse Type 2 diabetes!

How does Vitamin D3 Regulate Blood Sugar?
Because of the link between vitamin D3 and diabetes, researchers have sought to better understand the role of vitamin D3 on blood glucose metabolism. It was discovered that vitamin D3 upregulates the production of the glucose transporter GLUT4, which is responsible for taking up glucose from the blood. Therefore, vitamin D3 sufficiency may contribute to blood sugar regulation by promoting glucose uptake.
Taken together, these findings highlight the intriguing role of vitamin D3 for regulating blood sugar. Implying, getting sufficient sun exposure, and therefore vitamin D3, should be taken into consideration to help reverse Type 2 diabetes.
Enhancing Immune Function with Vitamin D3
The vitamin D receptor VDR is found in almost all immune cells, and explains why vitamin D3 has extensive effects on immunity. Here, we will explore how vitamin D3 sufficiency is essential for strengthening innate immunity, dampening chronic inflammation, and even modulating auto-immune conditions.

Vitamin D3 and Immune Defense
Vitamin D3 supplementation has been shown to contribute to the prevention of respiratory infections. This was highlighted during the pandemic, where vitamin D3 was utilized to help reduce the disease severity of COVID-19. In this case, vitamin D3 supplementation was found to improve disease symptoms and in some cases reduce the length of hospitalization. In contrast, vitamin D3 deficiency was found to be associated with increased mortality from COVID-19. These findings may explain why infections rise during winter months when sunlight is scarce, thus highlighting the prominent role of vitamin D3 for strengthening immunity.
How does Vitamin D3 Help Strengthen the Immune System?
In response to infection, vitamin D3 helps to clear invading pathogens by upregulating the production of antimicrobial peptides. For example, in monocytes, vitamin D/VDR activation of the CAMP gene increases the production of the antimicrobial peptide LL-37. LL-37 is a host-derived antimicrobial compound that kills invading bacteria, especially in the lungs. This suggests why sufficient vitamin D3 levels are important for preventing respiratory infections!
Despite vitamin D3’s ability to promote immune clearance of pathogens, it also exhibits potent anti-inflammatory effects. Though somewhat paradoxical, the reason vitamin D3 can exhibit both pro-inflammatory and anti-inflammatory effects simultaneously, is because the biological role of vitamin D3 is cell-type specific.
Anti-inflammatory Properties of Vitamin D3 - a role for Longevity
Although the role of sun exposure for longevity is often overlooked, vitamin D3 possesses strong anti-inflammatory properties which may prolong health span. As such, in fat cells, vitamin D3 downregulates genes which encode for inflammatory cytokines TNF-ɑ and IL-1. As a result, this reduces the production and secretion of pro-inflammatory cytokines, and instead promotes an anti-inflammatory environment. As chronic inflammation is a major determinant of biological aging, the anti-inflammatory properties of vitamin D3 emphasize the importance of sun exposure and (hence vitamin D3) for longevity.
Vitamin D3 and autoimmunity - Hashimoto’s Disease
Hashimoto's Thyroiditis (Hashimoto’s disease) is an autoimmune condition where the body produces antibodies against the thyroid, resulting in hypothyroidism. Although treatment for Hashimoto’s disease is effective, managing the disorder with lifestyle measures can be laborious. Fortunately, supplementing with vitamin D3 has been shown to improve Hashimoto’s disease through reducing the levels of antibodies responsible for destroying the thyroid. One study demonstrated that vitamin D3 supplementation was able to restore thyroid function in subjects with vitamin D3 deficiency and Hashimoto’s. This suggests that sufficient sun exposure, in combination with proper treatment, may help to manage the disorder.
Vitamin D3's Potential in Cancer Prevention and Therapy
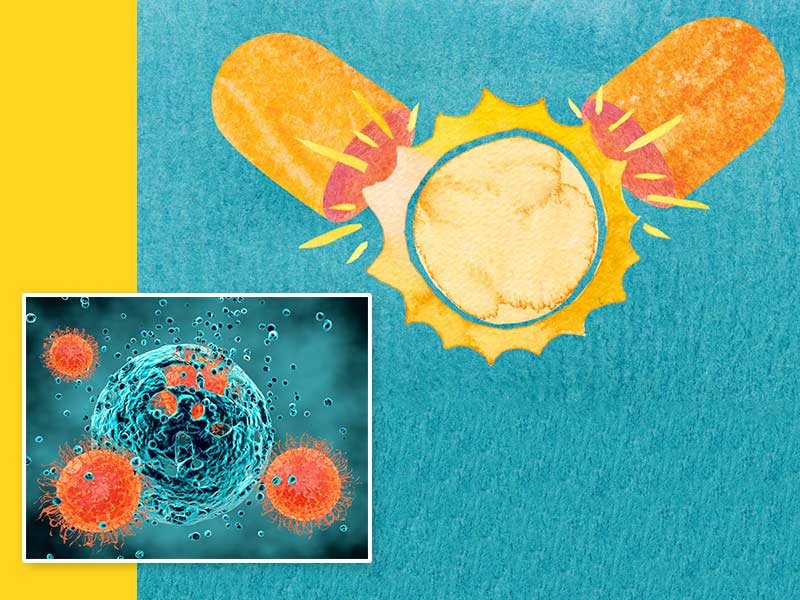
Cancer is a major cause of mortality worldwide, and is set to become more frequent in the population due to people living into old age. Although incredibly necessary, standard cancer treatments such as chemotherapy and radiotherapy are harsh on the body, and can increase the risk of additional morbidities such as infection. Therefore, some research groups have sought to discover if natural remedies can help prevent cancer growth, in addition to standard treatments.
Interestingly, vitamin D3 has been evidenced to influence the growth and proliferation of neoplastic (fast growing) cells including cancer cells. Emerging evidence suggests that because of this, vitamin D3 may play a role in preventing the development and progression of certain cancers.
Vitamin D3 and Colorectal Cancer (CRC)
In humans, a large percentage of cells in the colon express the vitamin D receptor VDR. Emerging data suggests that vitamin D3 supplementation may play a role in the prevention and progression of early stage colorectal cancer. Curiously, in colorectal cancer cell lines, vitamin D3/VDR has been shown to suppress genes involved in cell proliferation and migration such as MYC, thus preventing cell growth. Although colorectal cancer is a highly heterogeneous and a multifaceted disease, these results imply that vitamin D3 may exhibit anti-cancer effects in early-stage colorectal cancer by inhibiting pro-cancer genes.
Vitamin D3 and Improved Cancer Outcomes
Research suggests, in some cases, vitamin D3/VDR signaling might be linked to better cancer outcomes. Specifically, colorectal cancers expressing the VDR receptor have been evidenced to respond better to treatment, whilst aggressive colon cancers are often found to be VDR negative. In addition, vitamin D3 may further prevent cancer progression by modifying the tumour microenvironment. Meaning even in tumors that don’t express the vitamin D receptor, vitamin D3 may still contribute to preventing cancer growth by creating a surrounding environment that is non-favorable for cancer growth.
Disclaimer: Vitamin D3 supplementation alone is not a viable cancer treatment and shouldn’t be used as an alternative to chemotherapy.
Personalizing Vitamin D3 Supplementation for Health Optimization
Interestingly, research suggests people might respond to vitamin D3 differently. Called the Vitamin D Response Index (VDI), this may be useful to determine if you wish to personalise vitamin D3 intake for maximum health benefits.
If you wish to delve more into personalized healthcare, take a GlycanAge test to discover the health of your immune system, levels of chronic inflammation and biological age!
The Benefits of Vitamin D3: Summarized

Ultimately, vitamin D3 is critical for optimal health and wellness. This is signified by its ability to help with fat loss, regulate blood sugar, and even potentially prevent certain cancers. Incorporating sufficient sun exposure or supplementing with vitamin D3 is therefore essential to promote all-round health and longevity. If you could only take one supplement for the rest of your life, make it vitamin D3!
To discover how to maximize the benefits of vitamin D3, here are five supplements to combine with vitamin D3 to enhance its effects!
Maximizing Health Benefits: Supplements to Combine with Vitamin D3
The benefits of vitamin D3 are at large, calcium-dependent. This is because one of the main roles of vitamin D3 is to regulate calcium homeostasis. Meaning when you take both vitamin D3 and calcium together, they synergize to promote bone health.
When combined with vitamin D3, vitamin K2 is indispensable for ensuring calcium uptake is localised to the bones and teeth, and prevents it from accumulating in the vasculature.
Both vitamin D3 and omega-3s have anti-inflammatory properties. When taken together, they are synergistic, meaning their anti-inflammatory effects multiply to exhibit an even greater effect when combined. Tip! Look out for omega 3’s that are fortified with vitamin D3 for maximal benefits!
Due to its anti-inflammatory properties, vitamin D3 has been suggested to promote faster recovery after exercise. Interestingly, recent data has suggested that vitamin D3 supplementation might even promote muscle growth over fat gain in a caloric surplus. So whether you’re trying to aid recovery or grow some muscles, take your vitamin D3!
This powerful phytonutrient, found in broccoli and sprouted greens, has been shown to exhibit anti-cancer properties. Combine with vitamin D3 for the ultimate anti-cancer cocktail for optimal health.

