Hot Flashes And Menopause: Causes, Cures, And Quick Relief Methods
How to deal with hot flashes? Keep reading to discover handy hot flash remedies and effective treatments for hot flashes.
Summary:
- Hot flashes are the most common symptom of menopause, affecting around 80% of women.
- Symptoms of a hot flash include a sudden and intense surge of heat through the upper body, including the face, neck and chest, an elevated heartbeat, redness in the face and neck, and sweating. A chill often follows a hot flash episode as the body compensates for excess heat loss.
- Low hormones are believed to cause hot flashes, affecting the area of the brain that regulates body temperature.
- The frequency, severity, and duration of hot flashes vary from woman to woman and may be triggered by several factors.
- Discovering your true biological age with a GlycanAge test can provide vital information on the state of your health and how it relates to the severity of your hot flashes and other menopausal symptoms.
Introduction
If you’re going through menopause, you probably know all too well the predicament of a hot flash creeping up unannounced at the worst possible time. In these heated moments, many women feel at a loss for how to fight the fire within.
Hot flashes are the most common symptom of menopause and can range from mild, brief discomfort to being downright debilitating to your daily life. Wherever your hot flash symptoms fall within this spectrum, keep reading to learn about the causes and different treatments and medication for hot flashes, as well as useful tips that can help provide you immediate relief.
What Are Hot Flashes?
Hot flashes are characterised by a sudden and intense feeling of warmth in the upper body, predominantly around the face, neck, and chest, accompanied by a red, flushed face, rapid heartbeat and sweating. Many women report chills immediately after a hot flash due to losing excess body heat.
Hot flashes that happen at night are called night sweats and can cause sleep disturbances due to the intense heat surging through the body.
Hot flashes are vasomotor symptoms of menopause and affect around 80% of women. While the majority of women find them a minor inconvenience, for around 10-15% of them, symptoms can be so severe that they disrupt their everyday functions [1].

What Causes Hot Flashes?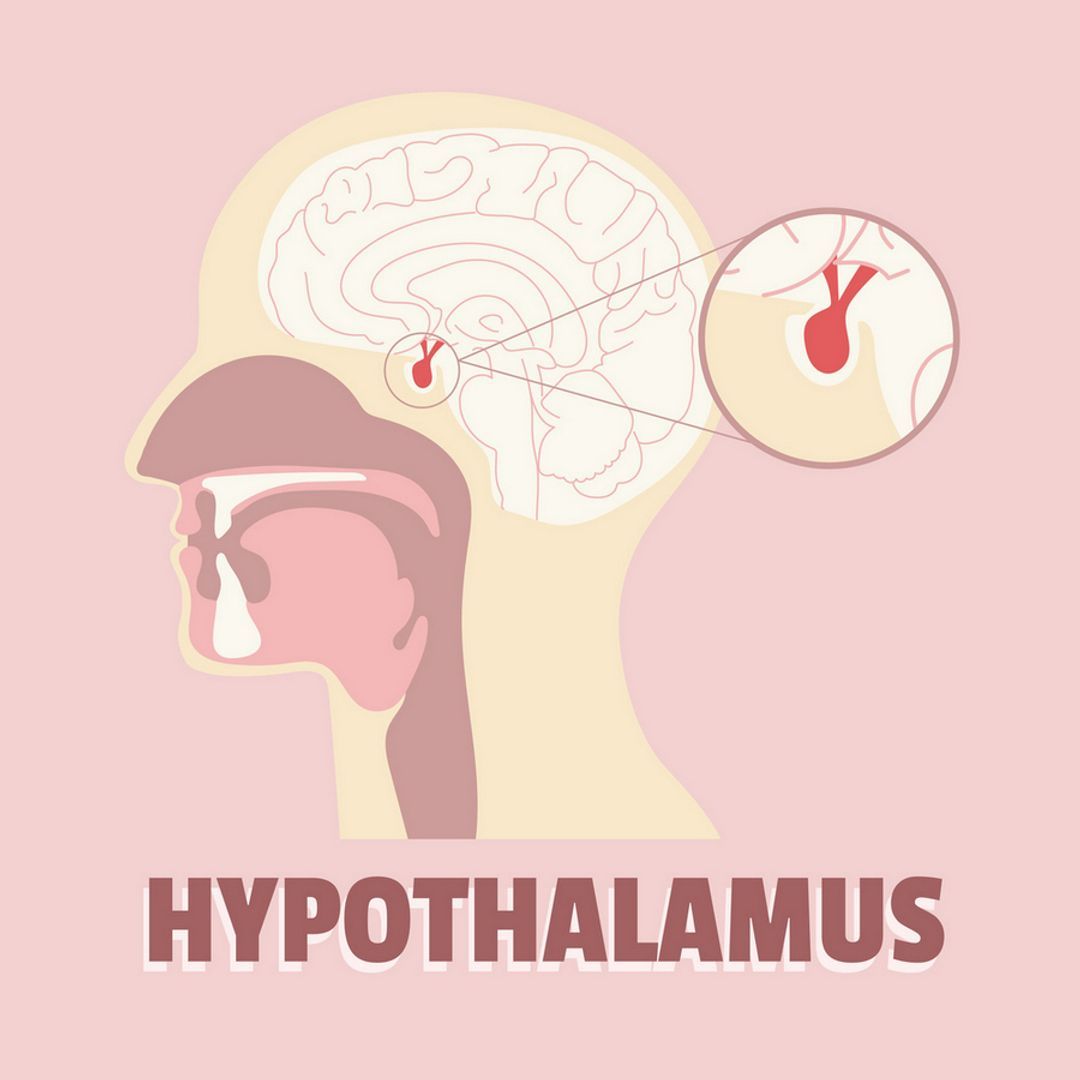
Though hot flashes are most commonly associated with (peri)menopause, they may also be a symptom of thyroid disease, infections, malignancy, as well side effects of some medications (e.g. antidepressants).
The exact mechanism and cause of hot flashes in relation to (peri)menopause have not been elucidated yet. What seems to happen is that with oestrogen levels dropping, chemical changes occur in the hypothalamus, which sits within the brain tissue and normally regulates body temperature [2].
As the body begins to heat up, the hypothalamus signals a chain of events throughout the body to bring the temperature back down. Blood vessels near the skin's surface widen to increase blood flow and help cool you down, causing redness and sweating. Heart rate may also increase, followed by a chill as the body compensates for excessive heat loss.
How Long Do Hot Flashes Last?
The frequency and duration of hot flashes vary substantially from woman to woman, and there is no reliable way to predict when they will begin and end. One episode may last less than a minute or even as long as ten minutes, but on average, they last around four minutes.
Additionally, there is no clear-cut answer on how many hot flashes per day are considered normal. While some women may experience one hot flash a week, others may have as many as 10 episodes a day.
Hot flashes can last anywhere between six months and eleven years or more following menopause, typically decreasing in frequency and severity over time. In a small proportion of women, they may never go away; however, the average time women experience hot flashes and night sweats is two years.
What Can Trigger A Hot Flash?
 Smoking
Smoking
According to one study [3], those women who smoked at any one point in their lives were 60% more likely to develop hot flushes compared to women that never smoked. This seems to be due to the effects nicotine has on the hypothalamus.
Obesity
A 2017 study by the North American Menopause Society found that high body mass index (BMI) is linked to a higher frequency of hot flashes because fat tissue acts as a strong heat insulator, making the distribution of heat more difficult [4].
Race
A 2013 study published in the American Journal of Epidemiology found that African-Caribbean and Hispanic women tend to be affected by hot flashes for longer than Caucasian and Asian women [5]. The racial differences in risk factors (including advanced age, obesity, smoking, and lower oestrogen levels) are thought to cause such disparity.
Stress
The surge in adrenaline and cortisol that kicks in during stressful ‘fight or flight’ moments can trigger a hot flash as a way of preparing for a perceived threat or danger.
 Caffeine
Caffeine
While research has produced conflicting results on the link between caffeine consumption and hot flashes, one 2015 study confirmed a positive correlation between caffeine use and more bothersome vasomotor symptoms in postmenopausal women [6].
Spicy foods
Spicy foods can elevate body temperature by dilating blood vessels and stimulating nerve endings, thus increasing the likelihood of experiencing more frequent and severe hot flashes.
Alcohol
While clinical evidence on the effects of alcohol in inducing hot flashes remains inconclusive, there is considerable anecdotal evidence to suggest that drinking red wine, in particular, does produce such effects.
It is believed that the stage a woman is at in her menopausal transition plays a role in this association, with some evidence indicating that alcohol use may lower hot flashes in peri-menopausal women [7].
 Heat
Heat
The likelihood of hot flashes is also increased when the outside temperature is warm or when engaging in strenuous activity.
Medication
Hot flashes can be a side effect of many prescription drugs, including opioids, osteoporosis medications, antidepressants, calcium channel blockers, steroids, and vasodilators. Speak to your doctor about alternative options if you suspect any medication you’re taking is exacerbating your hot flashes.
Tips On How To Ease Hot Flashes
Adopting certain lifestyle changes can provide quick relief for hot flashes when they unexpectedly strike without turning to prescription medications as a first resort.
Keep cool
Dress in layers, even on cold days, so you can easily remove items of clothing when a hot flash strikes. It’s also recommended to wear light, breathable, and loose-fitted clothing to help keep you cool.
Try carrying a portable fan or cooling spray with you throughout the day.
Sip on cold water and use ice packs or cold water wipes to cool your face, the back of your neck, and your chest in the midst of a hot flash.
For effective ways to deal with hot flashes at night, try layering a few blankets made of cotton, rather than a heavy-duty duvet, to help keep you cool and comfortable. You can crack open a window for a constant influx of fresh air or use a fan if you need to. Taking a cool shower before heading to bed can also help to bring down your body temperature.
Avoid triggers
It can take a while to figure out your triggers for hot flashes, but keeping a diary to record when an episode occurs can help you identify them. Whether it’s alcohol, caffeine, spicy food, or smoking cigarettes, it’s best to reduce your intake of such items or avoid them altogether to gain effective relief from your hot flashes.
If you’re taking medications known to cause hot flashes, review them with your doctor and discuss possible alternatives you can replace them with.
 Adopt diet and lifestyle changes
Adopt diet and lifestyle changes
Making healthy lifestyle choices can significantly reduce the frequency and severity of your hot flashes in the long term, as well as decrease the risk of other menopause-related diseases, including osteoporosis and heart disease.
Maintain a healthy weight by eating a balanced diet consisting of plenty of fruits, vegetables, healthy fats, and whole grains.
Incorporate foods high in plant oestrogen into your diet, such as chickpeas, lentils, soybeans, and flaxseed. Such foods contain isoflavones, a weak form of oestrogen that can reduce hot flashes.
Engage in a minimum of 30 minutes of moderate activity at least five times a week, including weight-bearing, resistance, and aerobic exercise. Try to exercise in a cool environment to avoid getting overheated and triggering a hot flash.
Try natural remedies
While studies are yet to confirm the benefits of natural remedies for hot flashes, many women find that certain herbal products can help in providing relief, including:
- Black cohosh
- Red clover
- Dong Quai
- Ginseng
- Wild yam
- Evening primrose oil
- Soy
However, these supplements aren’t without side effects; some can interfere with prescription medications and aggravate pre-existing health conditions. Moreover, due to a lack of regulation over their potency, purity and efficacy, such remedies aren’t recommended for long-term use. Don’t hesitate to speak with your doctor about these.
 Try alternative therapies
Try alternative therapies
A 2019 study published in the British Medical Journal found that five weekly 15-minute sessions of acupuncture significantly improved the severity and frequency of hot flashes in 80% of participants, rendering acupuncture a realistic option for women who cannot or do not wish to use prescription treatments [8].
Relaxation techniques like meditation and deep breathing can help you effectively manage your stress, which is often a trigger for a hot flash episode. In fact, one 2006 study that looked at menopausal women participating in a seven-week mindfulness-based stress reduction programme, found a 39% decrease in the frequency and severity of hot flushes, and a 28% improvement in their overall quality of life [9].
Prescription Treatment For Hot Flashes
If lifestyle and dietary changes, natural remedies, or alternative therapies aren’t enough to provide effective relief from hot flashes, or if they don’t subside naturally over time, you may need to turn to prescription treatments.
There are hormonal and non-hormonal options available; the type you choose depends on the severity of your symptoms as well as your past medical history, all of which your doctor can discuss with you beforehand.
Hormone replacement therapy (HRT)
 Taking the lowest effective dose of HRT for a limited time, preferably five years or less, can prevent or reduce the occurrence of hot flashes, as well as other menopausal symptoms such as vaginal dryness and mood swings.
Taking the lowest effective dose of HRT for a limited time, preferably five years or less, can prevent or reduce the occurrence of hot flashes, as well as other menopausal symptoms such as vaginal dryness and mood swings.
Oestrogen is the main hormone used to replace the body’s depleting levels in the form of gel, cream, patch, spray, implant or tablet. The treatment can be administered with or without progesterone, depending on whether you have your womb in place or not.
While HRT is the most effective way to stop hot flashes, it also comes with an increased risk of heart attacks, stroke, blood clots, breast cancer, and gall bladder disease; however, recent research suggests that newer formulations of HRT appear to carry a lower risk, particularly for women under 60 [10]. Your doctor will outline the benefits of HRT and outweigh them with the risks to determine whether it is the best treatment option for you.
It is important to note that hot flashes and other troublesome symptoms can return once you stop taking HRT, and the associated risks are highest in short-term patients.
If you are interested to know more about HRT, refer to our previous article here and feel free to discuss this option with your medical doctor.
Other prescription medications
Some women may not be able to or might choose not to take HRT. In such cases, non-hormonal alternatives are a reliable option, although they may not be as effective as hormonal therapy.
Antidepressants, such as fluoxetine, paroxetine, and venlafaxine, are approved as a treatment for hot flashes at a lower dose than that used to treat depression.
Other options include a blood pressure medicine called clonidine, a medicine used to treat urinary conditions called oxybutynin, and epilepsy medicines called gabapentin and pregabalin, which are normally prescribed for chronic pain and epilepsy. B complex vitamins and vitamin E supplements may also help, as well as ibuprofen, which are all available over the counter.
Every medication has its own side effect profile, so it is important to discuss this with your doctor in advance.
Nerve block procedure
Nerve blocking is a relatively new procedure that involves injecting an anaesthetic into the nerve cluster in the neck to treat moderate to severe hot flashes. The treatment has shown promise in providing relief to women who can’t take HRT and for whom prescription medications have not worked. Speak to your doctor for more information and to determine whether you qualify for this procedure.
What May You Consider Doing Next?
Menopause is a natural part of the ageing process, and while every woman will inevitably go through this transition, the severity and frequency of associated symptoms can differ significantly from woman to woman.
Discovering your biological age using our GlycanAge provides vital information on your current lifestyle and indicates whether there is room for improvement. This is to help optimise your health overall and will also help you navigate your menopause symptoms, including hot flashes.
Order your home testing kit today to get started.
FAQ
At what age do hot flashes start?
Hot flashes typically start in the perimenopausal stage when a woman first begins to experience irregularities in her monthly cycle. Usually, this transition starts between the ages of 45 and 55, with the average age being 51.
Do hot flashes ever go away?
Hot flashes do eventually subside; however, the length of time it takes varies from woman to woman. While some women take medication to prevent hot flashes, for others, they will naturally disappear without the need for treatment. In some cases, they may dissipate in as little as six months or last for up to ten years or more, but the average time for hot flashes is two years.
Are hot flashes harmful?
A 2019 study by the North American Menopause Society found that women who experience frequent and continuing hot flashes have double the risk of developing cardiovascular diseases, including heart attacks, strokes, and blood clots later on in life, compared to those who do not experience them at all.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459071/
- https://www.ncbi.nlm.nih.gov/books/NBK539827/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2673540/
- https://www.sciencedaily.com/releases/2017/05/170531084443.htm
- https://pubmed.ncbi.nlm.nih.gov/23788671/
- https://pubmed.ncbi.nlm.nih.gov/25051286/
- https://pubmed.ncbi.nlm.nih.gov/16087658/
- https://www.bmj.com/company/newsroom/acupuncture-may-ease-troublesome-menopausal-symptoms/
- https://www.webmd.com/menopause/news/20060913/meditation-may-cool-hot-flashes
- https://www.nice.org.uk/consultations/672/10/long-term-benefits-and-risks-of-hormone-replacement-therapy


