Do X-Rays Show Inflammation? Here’s the Answer
Can an X-ray show inflammation? What does an X-ray reveal? What are the pros and cons of X-rays? Click here to discover what shows up on X-rays.
Inflammation, the body's complex biological response to harmful stimuli, plays a crucial role in healing and defending against infection.
However, when this response persists longer than necessary, it can result in chronic inflammation, contributing to various diseases and conditions, including rheumatoid arthritis, heart disease and cancer.
Accurate detection and monitoring of inflammation are thus essential in guiding clinical decision-making and therapeutic strategies.
Among the numerous diagnostic tools available to physicians, X-ray imaging is one of the most frequently utilised techniques, primarily due to its accessibility, affordability and non-invasiveness.
However, the suitability of X-ray imaging for detecting inflammation has been a subject of debate owing to its inherent limitations in differentiating between various soft tissue densities.
This article delves into the capabilities of X-ray imaging in detecting inflammation while highlighting the nuances and limitations of this technique in diagnosing inflammatory conditions, as well as answers the question - how to reduce inflammation in the body fast?
What Are X-Rays?
 X-rays are a form of electromagnetic radiation with wavelengths shorter than visible light, enabling them to penetrate various materials, including human tissue. When X-rays pass through the body, they are absorbed by different tissues to varying degrees, depending on their density and atomic composition. As a result, a radiographic image is formed on a detector, capturing the contrasts between different tissue types.
X-rays are a form of electromagnetic radiation with wavelengths shorter than visible light, enabling them to penetrate various materials, including human tissue. When X-rays pass through the body, they are absorbed by different tissues to varying degrees, depending on their density and atomic composition. As a result, a radiographic image is formed on a detector, capturing the contrasts between different tissue types.
The image produced by an X-ray can be either analogue (photographic film) or digital, the latter offering increased sensitivity and improved contrast resolution, aiding in detecting subtle differences in tissue densities. However, the question remains: can you see inflammation on an X-ray?
What Does an X-Ray Show For?
X-ray imaging can indirectly detect certain inflammatory conditions, particularly those affecting the joints and bones. While X-rays cannot directly visualise inflammation, they can reveal changes in the tissues and bones that suggest an ongoing inflammatory process.
Some inflammatory conditions that X-rays can help identify include:
Rheumatoid arthritis
 X-rays can reveal signs of joint inflammation in rheumatoid arthritis, such as joint space narrowing, bone erosions and periarticular osteopenia (areas of low bone density around the joint).
X-rays can reveal signs of joint inflammation in rheumatoid arthritis, such as joint space narrowing, bone erosions and periarticular osteopenia (areas of low bone density around the joint).
Osteoarthritis
Although primarily a degenerative joint condition, osteoarthritis also involves an inflammatory component. X-rays can detect characteristic features, including joint space narrowing, osteophytes (bone spurs) and subchondral sclerosis (thickening of the bone beneath the cartilage).
Ankylosing spondylitis (AS)
 This chronic inflammatory condition affects the spine and sacroiliac joints, leading to the fusion of vertebrae over time. An X-ray of ankylosing spondylitis can demonstrate changes in the spine, such as sacroiliitis (inflammation of the sacroiliac joints), syndesmophytes (bony growths on the vertebrae) and vertebral fusion.
This chronic inflammatory condition affects the spine and sacroiliac joints, leading to the fusion of vertebrae over time. An X-ray of ankylosing spondylitis can demonstrate changes in the spine, such as sacroiliitis (inflammation of the sacroiliac joints), syndesmophytes (bony growths on the vertebrae) and vertebral fusion.
Gout
Gout is an inflammatory condition caused by the deposition of uric acid crystals in the joints. While X-rays cannot directly detect these crystals, they can reveal signs of chronic gout, such as joint space narrowing, bone erosions and periarticular tophi (deposits of uric acid crystals).
Inflammatory bowel disease (IBD)
In severe cases of IBD, such as Crohn's disease and ulcerative colitis, complications like bowel perforation, abscess formation or fistula development can be visualised through an abdominal X-ray.
Tuberculosis
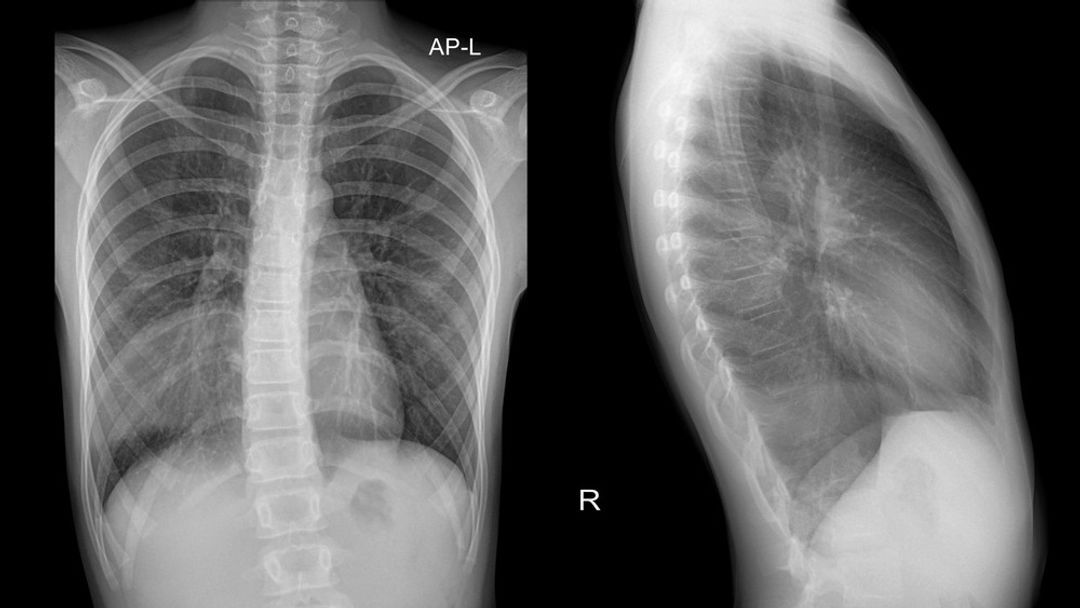 While not primarily an inflammatory condition, tuberculosis can cause inflammation in affected organs. X-rays, especially chest X-rays, can detect pulmonary tuberculosis by revealing characteristic features like cavitation, consolidation and pleural effusion.
While not primarily an inflammatory condition, tuberculosis can cause inflammation in affected organs. X-rays, especially chest X-rays, can detect pulmonary tuberculosis by revealing characteristic features like cavitation, consolidation and pleural effusion.
Pneumonia
X-rays can reveal areas of consolidation (whitish, dense regions) in the lungs, indicating inflammation and infection.
Lung cancer
Chest X-rays can reveal lung masses or nodules suggestive of cancer, although further imaging (e.g., CT scans) and tissue sampling are required to confirm the diagnosis.
Chronic obstructive pulmonary disease (COPD)
X-rays can show signs of emphysema (such as hyperinflation of the lungs and flattened diaphragms) or chronic bronchitis (e.g., increased bronchovascular markings) in patients with COPD.
Pulmonary oedema
Fluid accumulation in the lungs, often resulting from congestive heart failure, can be visualised on a chest X-ray as diffuse haziness, interstitial markings (Kerley lines) and an enlarged heart silhouette.
Cardiomegaly
An enlarged heart can be identified on a chest X-ray by assessing the size and shape of the heart silhouette, potentially indicating underlying heart conditions, such as hypertrophic or dilated cardiomyopathy.
Dystrophic calcification
This phenomenon occurs when calcium deposits form in injured or necrotic tissues as a result of chronic inflammation. The calcifications appear as dense, white areas on X-ray images and can be observed in several inflammatory conditions, such as:
Dermatomyositis (a rare inflammatory myopathy that affects the skin and muscles)
Systemic lupus erythematosus (SLE) (an autoimmune disease that can affect multiple organ systems)
Calcific tendonitis (inflammation of the tendons)
Calcinosis cutis (calcium salts in the skin).
 It is important to note that these X-ray findings indicate the consequences of inflammation rather than the inflammatory process itself.
It is important to note that these X-ray findings indicate the consequences of inflammation rather than the inflammatory process itself.
Additionally, X-rays may not be sensitive enough to detect early-stage inflammation or subtle changes in the affected tissues due to the technique's inability to differentiate between various soft tissue densities.
Inflammation often involves an increase in blood flow and swelling, which results in minimal contrast differences between the inflamed and adjacent healthy tissues. Consequently, X-ray imaging is limited in its capacity to directly identify the presence of inflammation.
In such cases, alternative imaging techniques like MRI, ultrasound or CT scans may offer better sensitivity and specificity in detecting and monitoring inflammation.
Pros and Cons of X-Rays
X-ray imaging is a widely used diagnostic tool in modern medicine, offering several advantages and some limitations. The benefits of X-ray imaging include the following:
Accessibility: X-ray machines are readily available in most healthcare settings, ranging from hospitals to outpatient clinics. As a result, X-ray imaging is often the first line of investigation for various medical conditions.
Affordability: Compared to other imaging modalities like MRI, CT or PET scans, X-rays are generally more cost-effective, making them a suitable diagnostic option, especially in resource-limited settings.
Speed: X-ray images are acquired relatively quickly, often within minutes. This rapid image acquisition makes X-rays valuable for time-sensitive situations, such as emergencies and urgent diagnostic evaluations.
Non-invasiveness: X-ray imaging is a non-invasive procedure requiring no surgical intervention or administration of contrast agents in most cases. This aspect makes it a preferable diagnostic tool for patients with contraindications to invasive procedures or contrast agents.
Good for bone imaging: X-ray imaging is highly effective for visualising bone structures, detecting fractures, dislocations and other bone abnormalities, as well as assessing the alignment and healing of bones.
 Despite its advantages, X-ray imaging has several limitations, including diagnosing inflammatory conditions:
Despite its advantages, X-ray imaging has several limitations, including diagnosing inflammatory conditions:
Limited soft tissue contrast: X-rays have limited sensitivity for differentiating between various soft tissue densities, making it challenging to visualise inflammation, masses or other soft tissue abnormalities directly.
Ionising radiation: X-ray imaging involves exposure to ionising radiation, which carries a small risk of harm, such as increased cancer risk with repeated or high-dose exposure. While the radiation dose is generally low, it is essential to minimise unnecessary exposure, especially in vulnerable populations like pregnant women and children.
Limited specificity: While X-rays can reveal certain changes in tissues and bones suggestive of inflammation, these findings may not be specific to a particular inflammatory condition. Further clinical and laboratory investigations may be required to establish a definitive diagnosis.
Quality and interpretation: The quality of an X-ray image can be affected by various factors, such as patient positioning, image acquisition settings and the skill of the radiographer. Additionally, interpreting X-ray images requires expertise, and subtle findings can sometimes be missed or misinterpreted.
Not suitable for all conditions: X-ray imaging is not ideal for assessing certain conditions, such as brain disorders, soft tissue injuries and early-stage joint inflammation, whereas alternative imaging techniques like MRI, CT scans or ultrasound may offer better sensitivity and specificity.
Alternative Imaging Techniques for Detecting Inflammation
Given the limitations of X-ray imaging in directly visualising inflammation, alternative imaging modalities are often employed for more accurate and sensitive assessment of inflammatory processes. Some of these imaging techniques include:
Magnetic Resonance Imaging (MRI)
 MRI uses powerful magnets and radiofrequency waves to create detailed images of the body's internal structures, providing excellent soft tissue contrast without exposure to ionising radiation. MRI can directly visualise inflammation and associated changes in the surrounding tissues, making it a valuable tool in diagnosing and monitoring various inflammatory conditions.
MRI uses powerful magnets and radiofrequency waves to create detailed images of the body's internal structures, providing excellent soft tissue contrast without exposure to ionising radiation. MRI can directly visualise inflammation and associated changes in the surrounding tissues, making it a valuable tool in diagnosing and monitoring various inflammatory conditions.
Ultrasound
Ultrasound imaging utilises high-frequency sound waves to generate real-time images of the body's internal structures. It is particularly effective in assessing soft tissues and can detect signs of inflammation, such as increased blood flow and swelling. Additionally, ultrasound is non-invasive, does not expose the patient to ionising radiation and can be performed at the point of care.
Computed Tomography (CT)
CT imaging combines multiple X-ray images taken from different angles to produce detailed cross-sectional images of the body. Although it still involves exposure to ionising radiation, CT can provide better soft tissue contrast than conventional X-ray imaging, potentially aiding in the assessment of inflammation.
Positron Emission Tomography (PET)
PET is a nuclear medicine imaging technique that can assess cellular metabolism and inflammation by detecting the distribution of radiolabeled molecules in the body (Townsend, 2008). PET imaging can directly assess inflammation and its response to therapy, making it particularly useful in managing inflammatory conditions.
Conclusion
X-ray imaging has long been a cornerstone of medical diagnostics, offering a quick, non-invasive and cost-effective window into the inner workings of the human body.
While its effectiveness in visualising bone structures and certain chest conditions is undeniable, the limitations of X-ray imaging in directly detecting inflammation and soft tissue abnormalities warrant careful consideration.
Inflammation, whether acute or chronic, often requires a more discerning eye, one that can pierce the veil of soft tissue densities and illuminate the subtle nuances of the inflammatory process.
Alternative imaging modalities, such as MRI, ultrasound, CT and PET, offer more accurate and sensitive assessments of inflammatory processes, enabling better diagnosis and monitoring of various inflammatory conditions.
By embracing the unique capabilities of these diverse imaging techniques, clinicians can navigate the complex landscape of inflammation with greater confidence, optimising patient outcomes and advancing the field of medicine.
Take Care of Your Health with GlycanAge
The GlycanAge biological age test is a cutting-edge diagnostic tool that offers insights into an individual's biological age, reflecting their overall health and ageing status more accurately than their chronological age.
 The best biological age test includes a personalised health assessment, monitoring the effects of lifestyle interventions and providing insights into inflammation and disease risk. Individuals who can benefit from the test include those looking to optimise their health, prevent age-related diseases or monitor the impact of lifestyle changes on their biological age.
The best biological age test includes a personalised health assessment, monitoring the effects of lifestyle interventions and providing insights into inflammation and disease risk. Individuals who can benefit from the test include those looking to optimise their health, prevent age-related diseases or monitor the impact of lifestyle changes on their biological age.
By offering a comprehensive understanding of an individual's health status, GlycanAge empowers people to make informed decisions about their well-being, enabling them to adopt personalised interventions and preventive strategies to maintain optimal health throughout their lives.
Once you receive your home testing kit, all you need to do is a simple finger prick test and send the results back to the lab. After 3-5 weeks of rigorous analysis to obtain the most accurate readings, your report will be ready.
You will also receive a complimentary 1-1 consultation with a scientist and/or healthcare professional to understand your results, devise an action plan to maintain or improve your biological age and optimise your overall wellness.
Several packages are available to buy, depending on your budget and where you are on your wellness journey. Start your wellness journey today - take our health quiz.
FAQ
Can an X-ray show muscle inflammation?
X-rays don't show soft tissue like muscle, so they are not a good tool for detecting muscle inflammation.
Can you see inflammation on an X-ray?
X-ray imaging can show certain inflammatory conditions, particularly those affecting the joints and bones. While X-rays cannot directly visualise inflammation, they can reveal changes in the tissues and bones that suggest an ongoing inflammatory process.
Do X-rays show inflammation intestines diverticulitis?
X-rays can't show diverticulitis. Blood and urine tests are considered a better option for diverticulitis.
Do chest X-rays show lung inflammation?
X-rays can show chronic lung conditions such as cancer.
Do X-rays show inflammation arthritis?
X-rays can reveal signs of joint inflammation in rheumatoid arthritis, such as joint space narrowing, bone erosions and periarticular osteopenia (areas of low bone density around the joint).


