One of the key questions in dealing with COVID-19 is how the same SARS-CoV-2 virus that causes mild to moderate symptoms in most individuals leads to very severe, sometimes even fatal disease in a subset of people. The overactivation of the immune system, often called the “cytokine storm” is believed to be an important factor. While standard reaction to the infection generates the level of inflammation sufficient to effectively wipe out the cause of the disease, cytokine storm is an exaggerated and uncontrolled release of the signals and molecules that not only harms the pathogens but also causes additional damage to our bodies.
Glycans attached to antibodies are an important regulator of our immune system, and they mediate signalling between other molecules and cells involved in our anti-viral response. For example, the attachment of a different glycan to the same antibody can convert it from an effector that activates the killing of the infected cell into an immunosuppressive mediator that dampens inflammation. Both functions need to be well balanced to adequately defend our bodies from the infection without causing additional harm. However, this fine-tuned process deteriorates with ageing, and as we are getting older our antibodies adopt a make-up of pro-inflammatory glycans that contribute to the development of age-related diseases through an increase of low-grade chronic inflammation termed inflammaging. However, this process of biological ageing is highly individual and levels of pro-inflammatory IgG can be very different in different individuals. Old age seems to be the predominant risk factor for severe COVID-19 disease, but since severe disease also develops in some younger adults, this opens the question about the role of IgG and plasma glycans in determining individual response to the infection with SARS-CoV-2 virus.
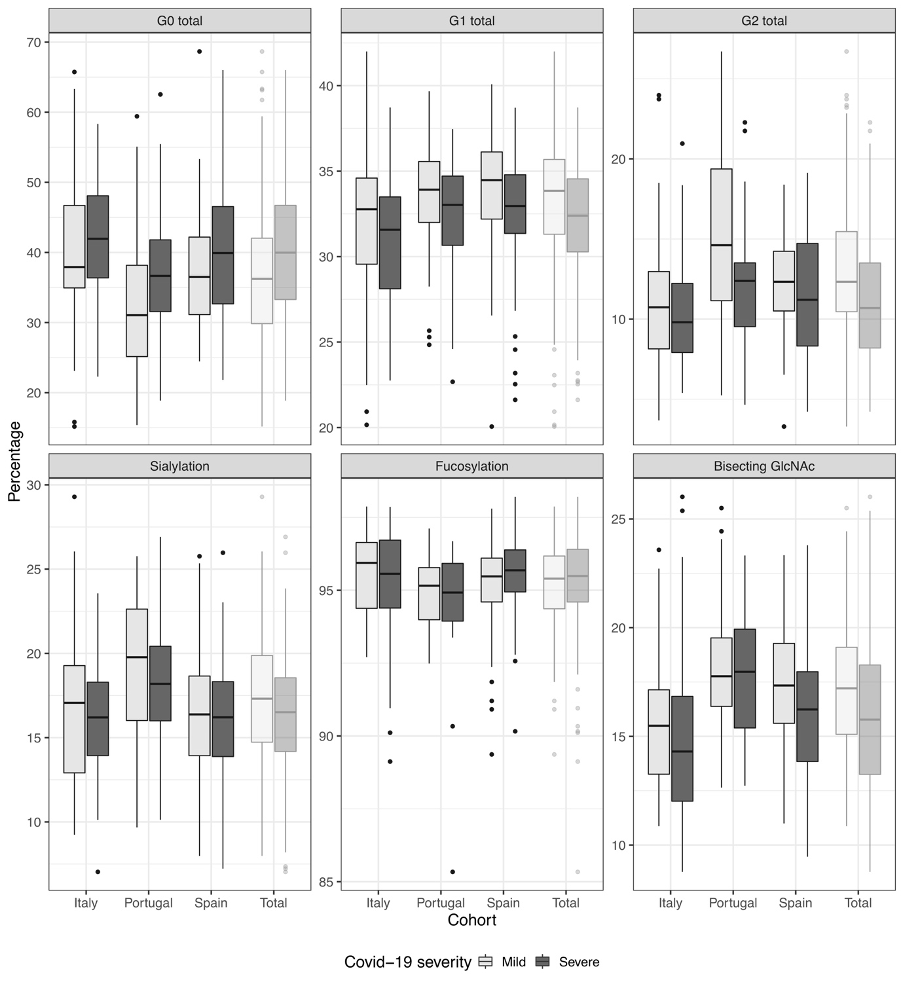
Just published study of 166 severe and 167 mild COVID-19 cases from hospitals in Spain, Italy and Portugal revealed statistically significant differences in the composition of the antibody glycome between mild and severe cases. The most notable difference was the decrease in bisecting N-acetylglucosamine (GlcNAc) in severe patients from all three cohorts. “Good glycans”, those that contain galactose and sialic acid were found to be decreased in severe cases in all cohorts, but this difference was not statistically significant after correction for multiple testing.
From this study alone, it is not possible to know whether the observed difference was a pre-existing risk factor or a part of the disease process. Therefore, additional studies in which the same person would be analysed several times in different stages of the disease are needed.
Relative abundance of main IgG glycome features in severe and mild COVID-19 cases from three cohorts.
G0 – agalactosylation, G1 – monogalactosylation, G2 – digalactosylation. Boxes represent the 25th and 75th percentiles. Lines inside the box represent the median.
Other articles you may like:
 Health
HealthGlycans as Drivers of a Disease Risk
The relative risk of many diseases increases with age. Individuals age at different rates, and while some might show a surprising level of health and fitness in their eight decades, others might be troubled by age-related diseases already in their late thirties. An increasing body of evidence suggests glycans play a role at establishing an individual’s risk of having poor health.

By Ph.D. Marina Martinic Kavur
 Health
HealthChanges of Glycans With Age in Different Parts of the World
Read how glycans change with age and lifestyle factors across the World.

By Prof Gordan Lauc, PhD
 Health
Health
 By Ph.D. Marina Martinic Kavur
By Ph.D. Marina Martinic Kavur