COVID-19 seasonality is an important open question with conflicting information from different studies. At the moment we see an apparent decrease in COVID-19 severity in most parts of the northern hemisphere, but it is still not clear whether the decrease in the number of seriously ill people is due to SARS-CoV-2 seasonality, or a simple consequence of the reduced number of infections due to social distancing. Most other coronaviruses show strong seasonal nature, but for SARS-CoV-2 there are millions of confirmed cases in warm and humid locations, which proves that virus can also be efficiently transmitted in warm and humid conditions.
However, besides its effects on viral transmission, warm weather may also improve the ability of people to fight the infection and prevent the development of severe disease. To address this question, we analysed individual patient’s records for 6,914 patients hospitalized in eight European and 15 Chinese hospitals since the start of the pandemics. With the onset of spring, a strong and statistically significant decrease in mortality was observed in all participating hospitals in Europe. The severity of the disease also decreased. Furthermore, the same pattern of changes was observed when we analysed individual symptoms reported by 37,187 participants of the COVID Symptom Study app in the UK.
After confirming that the decrease in COVID-19 severity and mortality was not caused by a change in the age distribution of hospitalized patients, we focused on the change in temperature and confirmed that the onset of spring is the most likely explanation for the observed changes. The increase in average temperature during hospitalisation for one-degree Celsius decreased mortality for approximately 15%, which could account for a significant part of decreased in COVID-19 mortality which we currently observe in most parts of the world. Unfortunately, this also paints a grim picture for the next winter, when more severe “winter” COVID-19 is expected to return - something we are currently observing in the southern hemisphere.
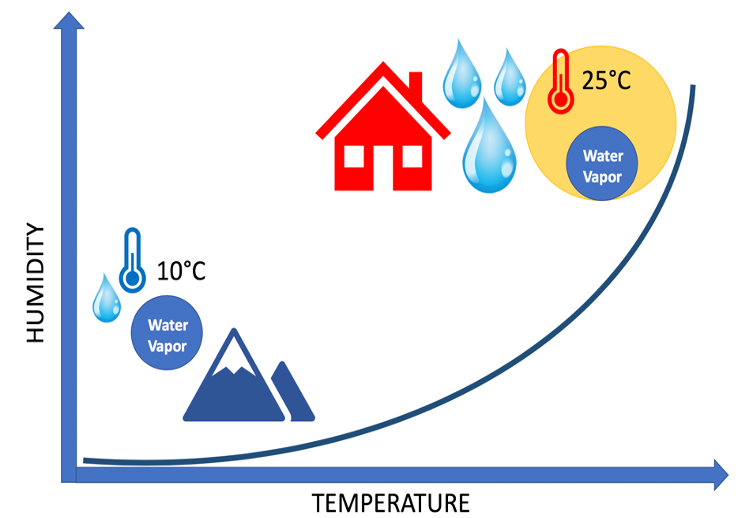
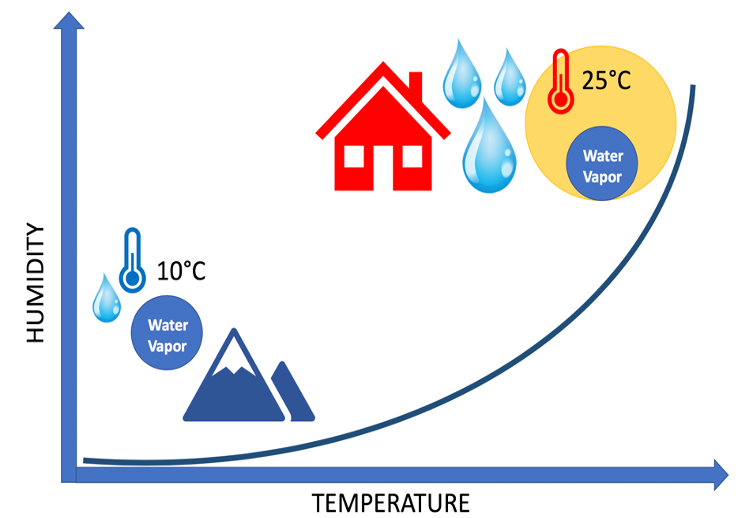
Molecular mechanisms that underlie the seasonal nature of respiratory viruses are dependent on two key elements: glycans and water. As I already explained in the Knowledge Hub article published in March Fighting Viruses with Glycans, our first line of defence against viruses is a special type of proteins called mucins that are secreted to our mucosal surfaces where they crosslink and inactivate viruses. However, this powerful barrier against viruses functions only when it is properly hydrated so that mucus can flow and remove viruses from our airways. In winter, unless air humidity is actively restored, heated indoor spaces often have a relative humidity of even below 20%, which is very low and inactivates our mucosal barrier by drying it out. This results in more severe COVID-19 in winter than what we are seeing at the moment. However, cooled indoor spaces may also result in very low relative humidity even in summer, which may also cause more severe COVID-19.
Complete manuscript presenting this study is available here.
Other articles you may like:
 Health
HealthEffects of Estrogens on the GlycanAge Index of Biological Age
Could hormone replacement therapy have an impact on your biological age? Read more about a recent study, addressing this question by analysing GlycanAge in 36 healthy premenopausal women.
Read full article  Health
HealthCan Glycans Predict the Loss of Kidney Function
Chronic kidney failure is one of the most common and debilitating complications of diabetes. Changes in glycosylation of immunoglobulin G (IgG) accompany biological agеing and regulates inflammation in diabetes – a process that participates in kidney function decline. A new study looks at the correlation between kidney function and IgG glycosylation.
Read full article  Health
Health