Post Menopause: Symptoms, Signs & Treatments

Get insights on managing symptoms and risks in the postmenopausal stage. Empower yourself with the knowledge to navigate this phase of life!
Summary:
Postmenopause is the last stage of menopause. It marks that a woman has stopped ovulating and hasn’t had a menstrual period for at least twelve months.
Hormones remain consistently low during postmenopause; as a result, women are at an increased risk of health conditions such as osteoporosis, cardiovascular disease, UTIs, and urinary incontinence, among others.
There are several ways women can gain relief from any postmenopausal symptoms they may be experiencing, ranging from dietary changes and increased exercise to taking supplements and seeking hormone replacement therapy.
Introduction
Menopause, there’s simply no escaping it. Every woman will experience a point in her life when her periods are coming to an end, and a whole host of other symptoms might appear. But while the effects of menopause are well-documented, not many women are aware of what happens after this stage.
There are around 13 million postmenopausal women currently in the U.K. aged 51 or above. This stage of life can bring in an entirely new set of symptoms for women. Keep reading to discover what happens after menopause, how long postmenopause lasts, the signs to look out for, and how to manage your postmenopausal symptoms effectively.
What Is Postmenopause?
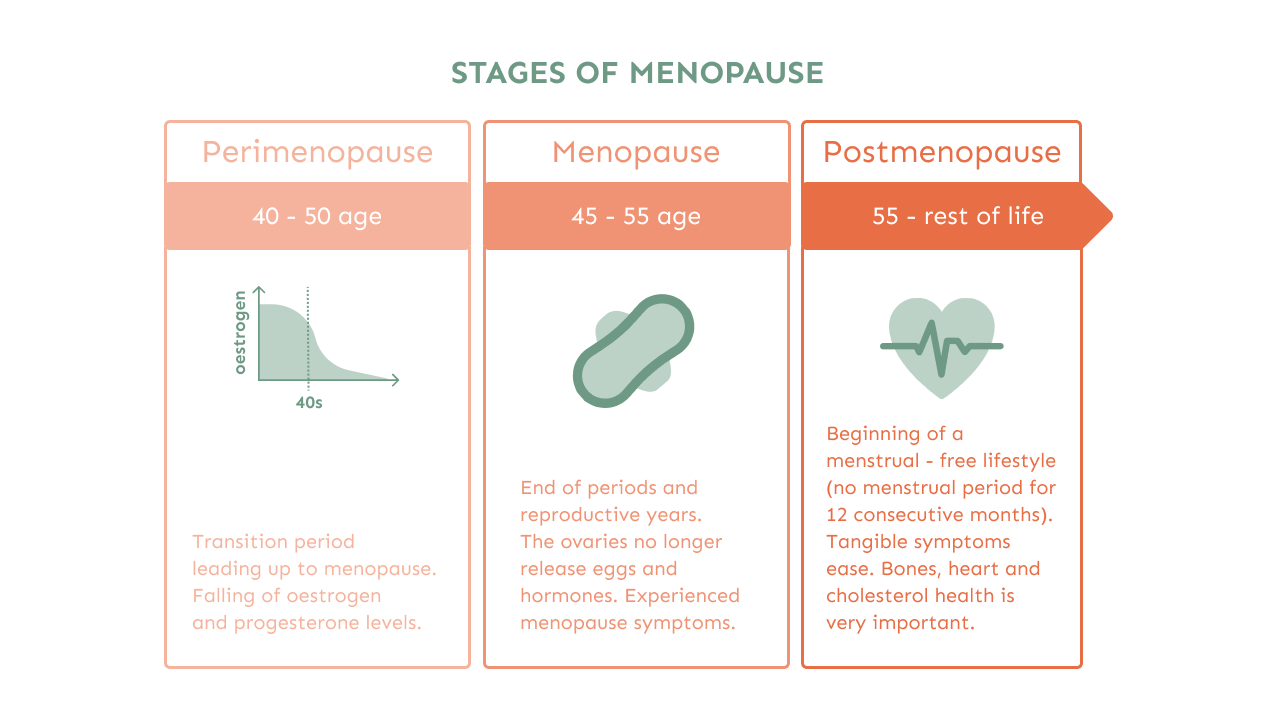
Postmenopause is the final part of a three-stage process, following perimenopause and menopause, when a woman stops ovulating and hasn’t had a menstrual period for twelve months or more.
During this time, some women will experience the lessening of symptoms typically associated with menopause, such as hot flashes, night sweats, and difficulty sleeping, however, other women, may find that the symptoms only worsen over time.
It’s also important to note that women are at an increased risk for conditions including osteoporosis, heart disease, depression, and vaginal dryness due to decreased postmenopausal hormone levels. It is, therefore, essential to take proactive measures to remain healthy.
How Do You Know When Menopause Is Over?
As mentioned above, being period-free for at least twelve months signals the end of menopause and the onset of postmenopause.
However, your healthcare provider can give you a diagnosis of postmenopause based on the date of your final period and your symptoms and by carrying out a simple blood test to check your hormone levels.
Your follicle-stimulating hormone (FSH) levels rise significantly during menopause as your ovaries begin to shut down. Having your doctor measure your FSH levels is currently one of the best ways to diagnose postmenopause.
What Happens During Menopause?
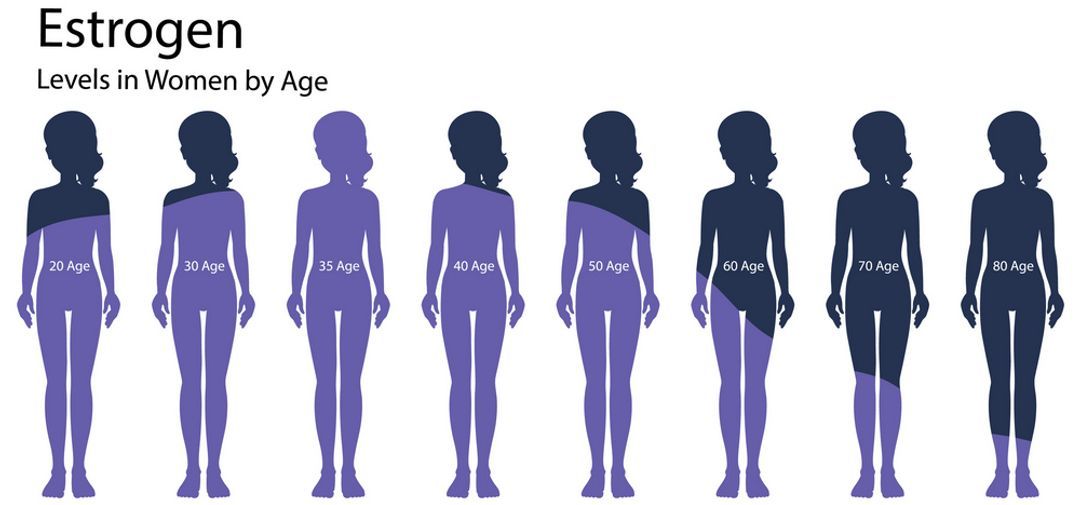
At this point, your hormones will remain at consistently low but stable levels, meaning you will no longer have a menstrual cycle or be able to fall pregnant because the ovaries have stopped releasing eggs and producing the sex hormones oestrogen and progesterone.
Despite the relief many women may feel being free from periods and the associated symptoms, low hormones can cause some side effects and increase the risk for certain health conditions.
How Long Does Postmenopause Last?
Once you enter postmenopause, you will remain in this stage for the rest of your life. Any symptoms that develop as a result can last, on average, around four to five years, although this period can be shorter or longer in different individuals.
This means that you will likely spend more years postmenopausal than you spent having your period. When you phrase it like that, you see the importance of understanding exactly what post-menopause will look like and how you can prepare.
Post Menopause Symptoms
With the drop in hormone levels, here’s a list of symptoms you can expect:
Thinning hair, brittle nails, and ageing skin
Thinning hair is a result of decreasing oestrogen and progesterone, as well as an increase in androgens, which cause the hair follicles to shrink. Androgens are also responsible for increased facial hair growth around the chin, jawline, and upper lip.
Your skin and nails need moisture to remain healthy, and because low hormones cause dehydration, it can leave your nails brittle and weak and your skin prone to dryness, wrinkles and fine lines.
Research shows that women lose around 30% of collagen during their first five years of menopause, after which they lose an average of 2% during the next 20 years due to declining oestrogen. As a result, skin loses its firmness and begins to sag, increasing the appearance of jowls, wrinkles and pores.
Weight gain
Declining hormone levels cause the body to store more fat around the abdomen and burn calories less efficiently. A slowing metabolism and sedentary lifestyle can also contribute to weight gain because of lower energy expenditure and a loss of muscle mass.
 So how to prevent menopause weight gain? With simple changes to your lifestyle - diet, exercise and sleep, you can combat this postmenopause symptom, but the key is to start early.
So how to prevent menopause weight gain? With simple changes to your lifestyle - diet, exercise and sleep, you can combat this postmenopause symptom, but the key is to start early.
Although exercise is always recommended, it is especially important for perimenopausal women to do some form of weight training, in order to increase muscle mass for better joint support.
Weight loss
While weight gain is a popular symptom of postmenopause, some women will end up losing weight. This can happen because of digestive issues, increased levels of stress and loss of muscle mass.
Vaginal dryness
Vaginal tissue becomes thinner and loses elasticity because of decreased collagen production, causing dryness, itching and a burning sensation - a condition known as vaginal atrophy. Vaginal atrophy affects more than half of postmenopausal women, often causing pain and discomfort during sexual intercourse.
This is just one of the ways sex changes during menopause, and you shouldn't be too shy to mention these symptoms to your GP.
Pain and discomfort during sex
As a result of vaginal dryness, some women may experience pain or discomfort during sex. Medically known as ‘dyspareunia’, this condition affects between 17% and 45% of postmenopausal women. Symptoms include tearing, bleeding, or spotting during or after penetrative sex as the vaginal walls become less elastic and more fragile.
Decreased libido
While vaginal dryness can lead to a lack of sexual desire, the fear or anticipation of painful intercourse can also trigger a decreased or total loss of libido as women experience performance anxiety and arousal problems. Using lubricants and topical creams is an effective way to make intercourse more comfortable.
Urinary Tract Infections (UTIs) and urinary incontinence
Oestrogen helps prevent infections by maintaining a healthy balance of the vaginal microbiome. So as oestrogen levels decrease, the risk of contracting UTIs subsequently increases. In addition, other factors such as weakening pelvic floor muscles also increase the risk of recurrent UTIs and urinary incontinence.
As a result, you may frequently experience sudden and strong urges to pee, urinary leakage, and difficulty completely emptying the bladder.
Adopting habits such as wiping from front to back, urinating after intercourse, taking showers instead of baths, and avoiding harsh soaps and hygiene products can help prevent recurring UTIs.
Mood swings and depression
 Emotions such as anger, irritability, anxiety and sadness are all common after menopause as hormones reach an all-time low, causing a knock-on effect on chemical reactions in the brain.
Emotions such as anger, irritability, anxiety and sadness are all common after menopause as hormones reach an all-time low, causing a knock-on effect on chemical reactions in the brain.
These hormonal dips can also trigger episodes of depression, particularly in women with a history of mental health issues. Research indicates that depression affects up to 1 in 5 women as they progress through menopause.
Osteoporosis
Because oestrogen directly affects bone composition, dwindling levels can cause them to become weak and brittle, a condition known as osteoporosis. In fact, you can lose up to 25% of your bone density after menopause, and around 1 in 10 women over 60 are affected by osteoporosis worldwide. Bones in the hips, wrists and spine are the most vulnerable to fractures.
Cardiovascular diseases
The risk for cardiovascular diseases, including heart disease, high blood pressure and stroke, also increase as women enter postmenopause and their oestrogen levels drop. The heart and blood vessels become more fragile and susceptible to plaque buildup during this stage.
Cardiovascular disease is the leading cause of death in women, affecting around 23,000 women each year. Research shows an increase in the incidence of heart attacks ten years after menopause.
Hot flushes and night sweats

While it was once widely believed that menopause-related hot flushes and night sweats faded after six to twenty-four months, now we know that these symptoms can persist for seven to eleven years after the menopausal transition.
The duration of time varies depending on factors such as ethnicity and lifestyle. For instance, women of Afro-Caribbean origin experience the longest duration of night sweats and hot flashes.
Luckily, there are ways to soothe these symptoms, to make sure your menopause hot flushes don’t ruin your quality of life.
Fatigue
Women experiencing hot flashes at night can vouch for how uncomfortable they can be, often preventing them from getting a good night’s sleep. Sleep disruption, paired with hormonal changes, can cause both physical and mental fatigue and might have a negative effect on overall well-being.
Enlarged breasts
If you’ve ever wondered - Why are my breasts getting bigger after menopause? we have the answer.
It can be the result of different factors - hormones, weight redistribution and genetics. During this transitional time, the drop in oestrogen levels causes milk glands to shut down, and the tissue becomes replaced by fat, leading to enlarged breasts.
We’ve already discussed post-menopause weight gain, but did you know that it can lead to breast growth due to weight redistribution? This means that excess fat tissue starts moving from other parts of the body into the breasts.
Your genetics could also lead to enlarged breasts, as you might be predisposed to it.
How Can I Manage Postmenopausal Symptoms?
Dietary changes
Eating a healthy, balanced diet that consists of plenty of fruits, vegetables, whole foods and healthy fats while avoiding processed foods that contain excessive salt and sugar is an effective way to achieve and maintain a healthy weight at this stage of life.
Dairy products like milk, cheese and yoghurt provide the body with nutrients such as calcium, magnesium, and vitamin D, which are essential for bone health. One study found that postmenopausal women who ate more dairy and animal protein had higher bone density than those who ate less. There is also evidence to suggest that dairy may promote deeper sleep in some menopausal women due to its glycine content.
Omega-3 fatty acids that are high in foods like oily fish, flax seeds, and hemp seeds can relieve the frequency and severity of hot flushes and night sweats, as well as reduce the risk of cardiovascular diseases, according to one review study of 483 postmenopausal women.
Whole-grain foods like brown rice and pasta, whole-wheat bread, barley, and quinoa, are high in fibre and B vitamins and have been linked to a reduced risk of heart disease, cancer and premature death.
Many studies confirm the benefits of colourful fruits and vegetables in alleviating a whole host of menopausal symptoms owing to their high vitamin, mineral, fibre and antioxidant content. In fact, one study of over 17,000 menopausal women found that women who incorporated more fruit and vegetables into their diet experienced a 19% reduction in hot flushes.
Certain fruits like dark berries and grapeseed extract supplements have been linked to improved sleep and reduced rates of depression. Such foods - in addition to chickpeas, peanuts, and black and green tea - are also high in phytoestrogens, which act as a weak form of estrogen in the body and may benefit postmenopausal health.
It is also beneficial for postmenopausal women to increase their intake of quality protein to offset the effects of decreased muscle mass and bone strength. Eating around 0.5 grams of protein per pound of body weight per day is recommended to maintain healthy muscle and bone density.
You should avoid spicy foods and alcoholic and caffeinated beverages as they can trigger and intensify hot flashes.
Stop smoking
Cigarette smoking is known to lower oestrogen levels, which can worsen the postmenopausal experience. Smoking can exacerbate symptoms and increase the risk of developing many medical conditions.

Consider Hormone Replacement Therapy (HRT)
HRT replaces the hormones that a woman’s body no longer produces after menopause.
HRT helps relieve menopausal symptoms, helps support your bones, prevents osteoporosis, and protects your cardiovascular system, amongst others. It is best to discuss this with your physician to find out if it would suit you.
Exercise daily
Engaging in at least 150 minutes of moderate activity each week, including weight-bearing, resistance, and aerobic exercise, can help slow bone loss after menopause and prevent weight gain. Regular exercise can also help lift your mood, improve sleep, and reduce hot flashes.
Take supplements in case of deficiency
There are various supplements that can help tame symptoms brought on by menopause. With advanced age, mineral and vitamin absorption are reduced, and it is worth checking your levels in case anything might need correcting.
For instance, a vitamin B6 supplement can help reduce energy loss and depression caused by low serotonin, while vitamin D and calcium supplements can reduce the risk of bone fractures in someone who is severely deficient.
Research indicates that your body loses its ability to absorb vitamin B12 as you age, resulting in a deficiency. Taking a B12 supplement or eating fortified foods can help with symptoms like fatigue, depression, weakness, and sluggish bowels.
Drink enough water
A lack of oestrogen affects the body’s ability to stay hydrated, and night sweats and hot flashes contribute to additional water loss. It is, therefore, important to drink around 8 to 12 glasses of water a day to help prevent dehydration and ease other symptoms like fatigue, weight gain, skin dryness, UTIs, and joint pain.
Have regular check-ups
Regular check-ups are a great way to ensure you are healthy and keep the risk of developing any chronic condition to a minimum. It is essential you attend available cancer screenings and smear tests and do not hesitate to contact your doctor about any unusual, persisting symptoms.
Different tests and screenings include:
- Pelvic exams
- Smear tests
- Mammograms
- Cancer screenings
- Bone density scans
- Immunisations

GlycanAge Test Can Help Ease Postmenopausal Symptoms
As women, we want to stay young for as long as possible, but it can often be challenging to evaluate how well your body is ageing and decide whether you need to make any lifestyle changes to slow down ageing.
But there is a solution!
A GlycanAge home test kit can give you an accurate estimate of your true biological age by examining the health of your immune system and the amount of inflammation in your body. The GlycanAge test reflects well on what is going on with your hormones. Thus you may use it as an aid if you are thinking about optimising your hormonal health using HRT or health in general by implementing a lifestyle intervention.
And the best part is that you can take this simple finger prick test without leaving your home! Just order a test kit, do the test at home, mail your sample to the lab, and wait for the results and your personalised consultation session!
FAQ
How long does postmenopause last for?
Hopefully a really long time. Postmenopause usually starts in your 50s and lasts for the rest of your life. Since postmenopause is such a long period of your life, it’s good to educate yourself about the symptoms and ways you can be proactive about improving your quality of life.
What age is post-menopause?
This is a very personal issue, on average women become postmenopausal in their 50s.
What are the symptoms of postmenopausal?
There are a lot of symptoms, but the variety and intensity will vary from woman to woman. The most popular postmenopausal symptoms are - thinning hair, weight gain/loss, vaginal dryness, discomfort during sex, decreased libido, UTIs, mood swings, osteoporosis, cardiovascular disease, hot flushes and night sweats, fatigue, and enlarged breasts.
What may I expect in postmenopause?
The majority of women do feel better once they have passed menopause because their hormones are now at a low but stable level. Debilitating menopausal symptoms tend to ease considerably, allowing women to experience a better quality of life with a more positive outlook.
With that said, some women may still feel the lingering symptoms of menopause for several years following their transition to postmenopause.
What are the signs that you need hormone replacement therapy?
If your menopausal symptoms become so severe that they’re adversely affecting your day-to-day life, it may be an indication to try hormone replacement therapy (HRT). HRT can help alleviate debilitating symptoms like depression, mood swings, vaginal dryness, bone weakness, hot flashes, and weight gain.
At what age should a woman stop taking hormone replacement therapy?
Experts generally recommend taking HRT in the lowest dose for the shortest time needed. Most women can stop taking HRT once their menopausal symptoms have ended, which is usually between two and five years. Deciding when to stop comes down to a decision that you make together with your doctor.

.png?alt=media&token=9cd45ebc-b13f-479f-952f-c700b6636f7b)

